The Differences and Similarities
As individuals age, hormonal changes become a natural part of life. Menopause in women and andropause in men are two significant stages that mark the end of reproductive years. Although these terms are often used to describe similar phenomena, it is important to recognize their unique characteristics.
Both menopause and andropause involve hormonal changes in the body. While menopause refers to the decline in estrogen and progesterone levels in women, andropause signifies a decrease in testosterone levels in men
While some men may experience symptoms of Andropause as early as their late 30s, the typical age range for andropause onset is between 40 and 55 years old. However, it’s important to note that hormonal changes during andropause occur gradually over time, and symptoms may become more pronounced with age.
Menopause, on the other hand, typically occurs in women between the ages of 45 and 55, with an average onset around 51 years old. However, perimenopause, the transitional phase leading up to menopause, can begin several years before the actual cessation of menstruation. Perimenopause, which can start in a woman’s late 30s or 40s.
- Estrogen (Women) and Testosterone (Men):
- Estrogen:
- Estrogen is a group of hormones primarily responsible for female reproductive development and function. It regulates the menstrual cycle, supports bone health, maintains vaginal lubrication, and contributes to the maintenance of healthy cholesterol levels.
- Testosterone:
- Testosterone is the primary male sex hormone, although it is present in both men and women. In men, it plays a crucial role in sperm production, sex drive, muscle and bone mass, red blood cell production, and overall well-being.
- Progesterone (Women):
- Progesterone is primarily involved in regulating the menstrual cycle and supporting pregnancy. It prepares the uterus for implantation, maintains the uterine lining during pregnancy, and helps regulate other hormones during the menstrual cycle.
- Hormonal Shifts during Menopause and Andropause:
- Menopause: During menopause, a woman’s ovaries gradually produce less estrogen and progesterone. This hormonal decline leads to the cessation of menstrual cycles, marking the end of reproductive years.
- Andropause: In men, andropause is characterized by a gradual decline in testosterone levels. While testosterone levels naturally decrease with age, andropause refers to a significant decline that may result in various physical and emotional changes.
Importance of Hormones in the Body:
Reproductive Function: Estrogen, progesterone, and testosterone play vital roles in reproductive health. They regulate fertility, support the development of reproductive organs, and influence the menstrual cycle and sperm production.
Bone Health: Estrogen and testosterone are crucial for maintaining strong and healthy bones. Estrogen helps in the absorption of calcium and other minerals, preventing bone loss and reducing the risk of osteoporosis. Testosterone also contributes to bone density and muscle mass in both men and women.
Sexual Function: Estrogen and testosterone significantly impact sexual health. Estrogen helps maintain vaginal lubrication, elasticity, and sensitivity, while testosterone is essential for sexual desire and erectile function in men.
Metabolism and Body Composition: Hormones influence metabolism, body composition, and fat distribution. Estrogen and testosterone help regulate metabolism, body fat distribution, and muscle mass, impacting overall body composition.
Mood and Emotional Well-being: Hormones influence brain chemistry and play a role in mood regulation. Changes in hormone levels during menopause and andropause can contribute to mood swings, irritability, anxiety, and depression.
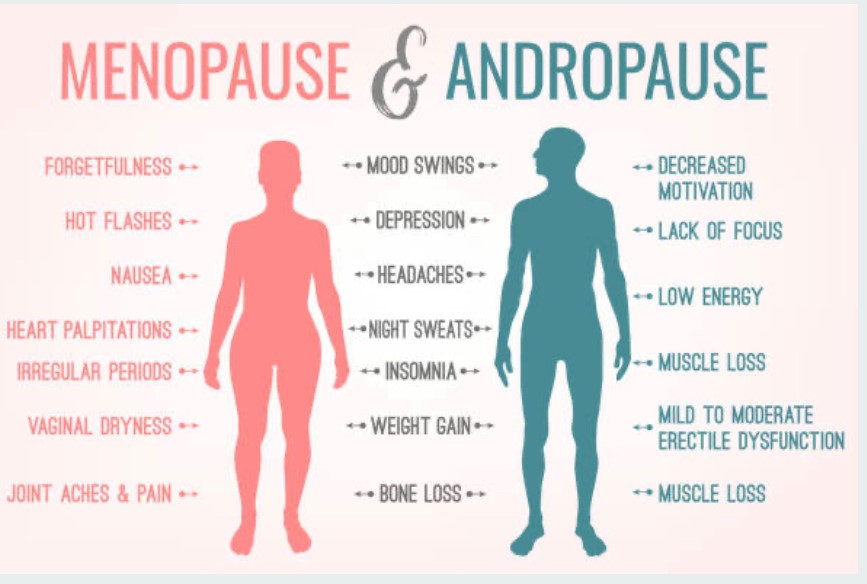
Physical symptoms of Menopause
- Hot flashes: Sudden feelings of intense heat, often accompanied by sweating and flushed skin .
- Night sweats: Excessive sweating during sleep, leading to damp bedding and disrupted sleep.
- Vaginal dryness: Reduced vaginal lubrication, resulting in discomfort or pain during intercourse.
- Sleep disturbances: Insomnia, night awakenings, or difficulty staying asleep.
- Changes in menstrual cycle: Irregular periods, shorter or longer cycles, or eventually the complete cessation of menstruation.
- Urinary changes: Increased frequency of urination or urinary incontinence.
- Changes in skin and hair: Skin may become drier, thinner, and more prone to wrinkles. Hair may become thinner and drier.
- Weight gain: A tendency to gain weight, particularly around the abdomen.
- Reduced bone density: Increased risk of osteoporosis and fractures due to decreased estrogen levels.
Physical Symptoms of Andropause:
- Erectile dysfunction: Difficulty achieving or maintaining erections, reduced sexual desire, or decreased quality of erections
- Reduced muscle mass: Loss of muscle mass and strength, leading to decreased physical performance.
- Fatigue: Persistent feelings of tiredness, reduced energy levels, and decreased stamina.
- Increased body fat: Shift in fat distribution, with more fat accumulating in the abdominal area.
- Hair loss: Thinning of hair, particularly on the scalp.
- Sleep disturbances: Disrupted sleep patterns, including insomnia or restless sleep.
- Reduced bone density: Decreased bone density and increased risk of osteoporosis.
- Decreased fertility: Reduced sperm production and motility, leading to decreased fertility.
- Changes in cholesterol levels: Alterations in lipid profiles, including increased levels of LDL cholesterol and decreased levels of HDL cholesterol.
Psychological Impact of Menopause:
Mood swings: Women may experience frequent mood swings, including irritability, sadness, anxiety, and feelings of being overwhelmed.
Depression and anxiety: Hormonal fluctuations during menopause can contribute to the development or exacerbation of depression and anxiety disorders.
Cognitive changes: Some women may experience memory lapses, difficulty concentrating, and reduced cognitive function during menopause.
Fatigue and sleep disturbances: Sleep disturbances, such as insomnia or disrupted sleep, can lead to fatigue, which can impact mood and overall well-being.
Decreased self-esteem: Physical changes, such as weight gain or changes in body shape, may affect self-esteem and body image.
Psychological Impact of Andropause:
Irritability and mood changes: Fluctuating hormone levels can lead to increased irritability, mood swings, and a general sense of dissatisfaction.
Fatigue and decreased motivation: Men may experience persistent fatigue, reduced energy levels, and a lack of motivation.
Depression and anxiety: Hormonal changes during andropause can contribute to the development of or increased vulnerability to depression and anxiety.
Cognitive changes: Some men may experience difficulty concentrating, memory problems, and reduced cognitive function during andropause .Decreased self-confidence: Physical changes, such as hair loss or decreased muscle mass, can impact self-confidence and body image.
Although menopause and andropause are distinct processes that occur in women and men, respectively, they can have an impact on the dynamics of interpersonal relationships, particularly within a romantic partnership. Here are some considerations regarding the potential interaction between menopause and andropause:
Shared Understanding:
When both partners are experiencing hormonal changes simultaneously, there may be a greater level of empathy and understanding between them. Recognizing and acknowledging each other’s symptoms and challenges can foster compassion and support within the relationship.
Communication:
Open and honest communication is crucial during this phase. Discussing the physical and emotional changes experienced during menopause and andropause can help both partners navigate the challenges together. Sharing concerns, seeking reassurance, and expressing emotional needs can foster mutual understanding and strengthen the bond.
Intimacy and Sexuality:
Both menopause and andropause can impact sexual desire, function, and satisfaction. It is important for partners to communicate their needs, concerns, and any physical changes they may experience. Exploring alternative ways to maintain intimacy and sexual connection, such as trying new activities or seeking professional advice, can help adapt to the changes and maintain a satisfying and fulfilling sexual relationship.
Emotional Support:
The emotional impact of hormonal changes can affect both partners. Providing emotional support, being patient, and validating each other’s feelings can help alleviate stress and foster emotional well-being. Engaging in activities that promote relaxation and stress reduction, such as practicing mindfulness or exercising together, can also contribute to emotional balance
Seeking Professional Help:
In some cases, the challenges posed by menopause and andropause may require professional assistance. Couples therapy or individual counseling can provide a safe space to address concerns, enhance communication skills, and develop coping strategies that support the relationship throughout this transitional phase.
It’s important to remember that every relationship is unique, and the impact of menopause and andropause will vary among couples. By maintaining open lines of communication, seeking support when needed, and approaching these changes as a shared journey, couples can navigate through menopause and andropause with understanding, empathy, and love.
menopause, andropause, menopauseandandropause, menopauseandsexuality, whatisandropause, whatismenopause, menopausematter, gilliannefuller. blogsbymenopausematter, perimenopause, postmenopause, aginggracefully, estrogen, testosterone, progesterone, menopauseeducation, menopausesupport